Niemann-Pick type C disease has serious consequences for those who have it. Early diagnosis, symptomatic treatment, and a substrate inhibitor can help these patients until there is a cure.
Niemann-Pick type C disease is an inherited disease that affects lipid metabolism, that is, how fats, lipids, and cholesterol are stored in the body or are eliminated. In patients with Niemann-Pick disease, abnormal lipid metabolism causes the accumulation of lipids at a harmful level in various organs. The disease mainly affects the liver, spleen, bone marrow, and brain. Most often, the telltale signs of the disease are absent at birth. They only appear after a period of evolution of a few months, several years, or even adulthood.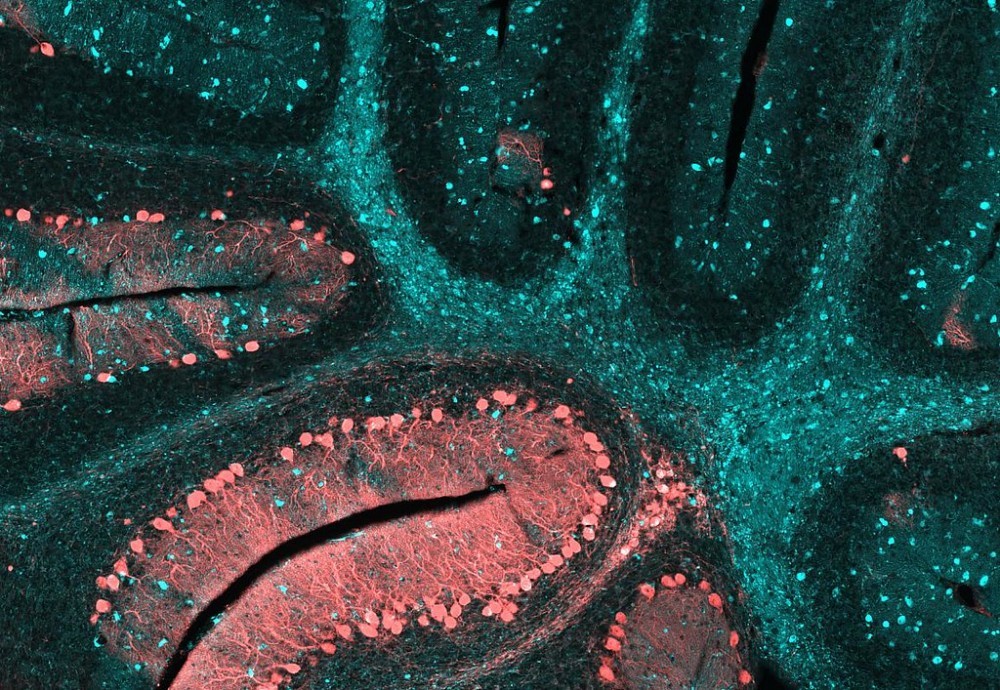
People with the disease carry a genetic mutation that is manifested by the abnormal accumulation of cholesterol in a particular compartment – called the lysosome – inside the cells.
Cholesterol accumulates in the liver and spleen, which causes various complications: liver and respiratory disorders, poor coordination of movements (ataxia), visual disturbances … In adults, it manifests itself mainly in psychic and neurological disorders.
NPC, which affects about one in 100,000 to 150,000 children, is a disease that is often misdiagnosed and/or under-diagnosed. Patients with the disease usually have ataxia in infancy, progressive impairment of motor and intellectual function, and often die before adulthood.
*** Lysosome and Niemann-Pick Type C Disease
Located at the heart of each of our cells, the role of the lysosome is to recycle materials – called metabolites – resulting from cell function. It contains all the substances necessary for the transformation of large molecules into smaller units that the body can then either reuse or eliminate.
Each protein is involved in a metabolite. These proteins are responsible for either the degradation of the metabolite or its transport. A gene defect causes either a non-production of the corresponding protein or its dysfunction. The metabolite concerned is then no longer or poorly supported in the lysosome and accumulates. The cells will gradually become engorged and the different organs will not function normally.
This accumulation will cause the appearance of lesions in different organs causing particularly serious and irreversible disorders.
*** Glycans and Niemann-Pick Type C Disease
Glycans are sugar molecules, which envelop each living cell in the human body. These complex carbohydrate chains fulfill a multitude of vital functions, providing the machinery needed for communication between cells, to reproduce and survive. They normally undergo some kind of recycling process when they enter the cell so that they are recharged and ready to work when they return to the surface.
Alteration of cholesterol trafficking in cells leads to poor recycling of glycans on the surface of the cell. Patients with NPC are unable to metabolize cholesterol, the waxy substance builds up in the brain and leads to neurodegeneration. Glycans are stuck inside the cell making communication and transport for these cells difficult or impossible.
*** Esterified Cholesterol
There are two chemical forms of cholesterol:
– Cholesterol in free form – not bound to another substance. It is transported in the blood by the light-weight lipoproteins, LDL.
– Cholesterol esterified, that is to say, combined with fatty acid – to form sterids.
Esterified cholesterol (together with an essential fatty acid) is transported to the cell lysosome by heavy-weight lipoproteins, HDLs – molecules formed from proteins and lipids -. It hydrolyzes by releasing LDL and, once free (unesterified), it leaves the lysosome and can be used in membrane biosynthesis or re-esterified to be stored in the cell.
*** Why Are These Diseases Genetic?
A genetic disease is due to a mutation (misspelling) that can occur in the sequence of letters that make up the sequence of a gene. This results in the manufacture of an abnormal protein or its absence.
*** Why Are These Diseases Hereditary?
In the parents of sick individuals, an altered copy of the gene involved in the disease, that is to say with a “misspelling” (mutation), is found in all the cells as well as in a number of their sexual cells (spermatozoon or ovum).
Just like normal genes, the altered gene can be passed from parents to children.
I – Causes of Niemann-Pick Type C Disease
Niemann-Pick type C disease is a lysosomal neurodegenerative disease linked to a genetic mutation in chromosome 18, involving the mutation of the NPC1 gene in approximately 95% and the mutation of NPC2 in approximately 4% of cases.
It is essentially associated with the body’s inability to effectively eliminate excess cholesterol and other lipids. If it is not broken down properly, cholesterol builds up in the spleen and liver, and excessive amounts of other fats accumulate in the brain.
Alteration of lipid transport results in a massive accumulation of non-esterified cholesterol and glycolipids, particularly sphingolipids in neurons, due to a lack of intracellular cholesterol utilization.
II – Symptoms of Niemann-Pick Type C Disease
1 – Possible Symptoms of Niemann-Pick Type C Disease:
– Hepatomegaly: Liver disease, jaundice (yellowing of the skin after birth).
– Splenomegaly: Abnormal enlargement of the spleen.
– Hypotonia: Decreased muscle tone.
– Dysmetry: Inability to correctly adjust the intensity or duration of an action (too much abruptness, too much speed, too much amplitude, etc.).
– Dysphagia: Swallowing disorders.
2 – Typical Neurological Signs of Niemann-Pick Type C Disease Are:
– Cerebellar ataxia: Loss of balance, difficulty walking or clumsiness, difficulty moving limbs.
– Dysarthria: Disorders of the speech.
– Dystonia: Involuntary muscle contractions.
– Supranuclear Ophthalmoplegia: Difficult to move the eyes (especially from top to bottom).
Symptoms of Niemann-Pick Type C Disease usually begin to appear in children around the age of five.
However, it can occur at any stage of life, from birth to adulthood.
Hepatic disorders or unchanged hepatosplenomegaly may be the first signs of the disease, but its seriousness comes from the subsequent neurological manifestations that are due to the accumulation of sphingolipids in the nerve cells.
In the small child, one can note hypotonia. A little later, the patient may experience dystonia, ataxia, dysarthria, and cognitive impairment. Seizures or cataplexic seizures can also occur. Supranuclear vertical and horizontal paralysis of the gaze is very often found in children. Swallowing disorders may require gastrostomy to avoid false roads.
These signs are inevitably aggravated, ultimately leading to patient dependence.
When the disease appears only in adolescence or adulthood, the visceral signs are almost always absent. The psychiatric signs are then predominant, depression, psychosis, or even dementia, possibly accompanied by neurological signs.
In general, very early forms lead to death in childhood or adolescence, whereas late forms, with less severe clinical signs, make it possible to reach adulthood.
Although difficult to establish, the prognosis depends on the age of the first neurological symptoms and their evolution, in particular, the speed of progression and any associated complications.
III – Diagnosis of Niemann-Pick Type C Disease
The disease is usually diagnosed by a skin biopsy. Once the sample is taken, lab technicians analyze skin cells for growth and see how they evolve and store cholesterol. A doctor may also use DNA tests to look for the genes that cause the disease. The diagnosis is made by highlighting these abnormalities – in particular by the test with filipine – in fibroblasts in culture.
Filipin is a synthetic antibiotic that has the ability to unite with free cholesterol by forming a complex that after being illuminated with ultraviolet light emits fluorescence.
Prenatal diagnosis is easier by molecular biology but can also be done by cell biology.
The neurological signs make it serious and make it possible to differentiate several forms:
– The infantile form (20%) begins around 12-18 months by a delay of the motor development associated with hypotonia, then the loss of the motor acquisitions. The evolution is towards a pyramidal syndrome and a bedridden state. Death occurs between 3 and 6 years.
– The late infantile form (30% of cases) begins around 2-5 years old with ataxic walking. Death occurs for around 10 years.
– The juvenile form (30% of cases) begins around 6-12 years old by academic difficulties or epilepsy or cataplexy attacks or ophthalmoplegia. The evolution is towards a pyramidal syndrome, a bedridden state, psychotic episodes. Death occurs in the 2nd decade.
– The adult form (20% of cases) whose symptomatology is close to that of the juvenile form with significant psychiatric disorders.
IV – Treatment of Niemann-Pick Type C Disease
The drugs used are symptomatic or palliative to treat neurological disorders: anticholinergic, botulinum toxin for dystonia and tremors; antiepileptics; tricyclic antidepressants and psychostimulants for cataplexy; painkillers.
A drug called miglustat is currently used to treat the disease. It is classified as an enzyme inhibitor and works by preventing the body from producing fatty substances to limit their accumulation.
Continuation of treatment should be re-evaluated after at least 1 year of treatment. The most common adverse events are diarrhea, weight loss, and tremors. This medicine is subject to hospital prescriptions.
Non-drug management includes dietetic/nutritional care, speech therapy, physiotherapy, psychological assistance, or psychiatric care.
V – Research on Niemann-Pick Disease
1 – Discovery of a Drug That Accelerates Cellular Recycling
A team of biologists from the University of Michigan in a study published in the journal Nature in April 2012, identified a potential drug that accelerates the disposal of waste from the cell recycling center, the lysosome.
The researchers believe that it is possible to use ML-SA1 as a drug to activate the lysosome calcium channels and restore the normal functioning of the lysosome in lipid memory diseases like Niemann-Selection. The same approach could also be used to treat neurodegenerative diseases affected by defects in lysosome trafficking such as Alzheimer’s or Parkinson’s diseases.
2 – Discovery of a Substance Releasing Cholesterol Trapped in Cells
In a study of the Southwestern Texas University published in the Annals of the American National Academy of Sciences (PNAS) in 2009, researchers identified in mice a substance that releases excess cholesterol accumulated in cells.
This discovery sheds light on how cholesterol is transported into the cells of our body and could pave the way for therapy for Niemann-Pick type C disease.
The researchers showed that very quickly after injection of the substance called CYCLO (2-hydroxypropyl-beta-cyclodextrin), a huge amount of cholesterol accumulated in the cells was suddenly released before being metabolized normally. With only one dose, they achieved the excretion of one-third of the abnormal accumulation of cholesterol in these cells.
These researchers made a single CYCLO injection in seven-day-old mice that were induced by Niemann-Pick Type C disease. Shortly thereafter, these mice began to metabolize cholesterol normally.
After 49 days, these mice continued to have significantly lower cholesterol levels in their tissues than control animals not treated with CYCLO. Their liver functions also improved and they also experienced less neurodegeneration.
The results of this research show that researchers have apparently overcome the lack of transport of cholesterol in cells due to genetic variation and which explains its abnormal accumulation but they still do not understand what is happening at the molecular level.
The next step is to determine the dose of CYCLO needed to trigger the release of all accumulated cholesterol. They also hope to determine the life expectancy that CYCLO achieves in treated mice and the duration of the effects of this treatment.
3 – Clinical Study Around the Drug Vts-270 for the Treatment of the Disease
In 2015, the National Institutes of Health (NIH) launched a second clinical trial on the development of VTS-270 for the treatment of NPC, designed to evaluate the efficacy of the compound for its treatment.
The VTS-270 has been shown to be a promise in preclinical and clinical studies as a treatment for the disease. It consists of a well-characterized mixture of 2-hydroxypropyl-beta-cyclodextrin, which has been widely evaluated in preclinical and clinical studies at the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Child Health and Human NICHD. Development) and the NIH Clinical Center.
4 – Bortezomib, a Possible Therapy for Niemann-Pick Type C Patients
In a study published by the Niemann-Pick Foundation of Spain in January 2014, researchers presented Bortezomib as a possible therapy for Niemann-Pick type C patients with nonsense mutations.
Currently, about 300 mutations in the NPC1 gene are described as the cause of 95% of patient cases, the majority of which are nonsense.
Some mutations prevent the correct folding or assembly of proteins. The misfolded proteins are recognized by a quality control mechanism, known as ERAD, which allows the output of the endoplasmic reticulum to only proteins with correct wrinkling. Thus the cells make sure that only mutant proteins arrive at the corresponding cellular compartment where they will perform their function correctly.
NPC patients with nonsense mutations can be treated with proteasome inhibitors, thereby slowing the progression of the disease and improving their quality of life.
There is a proteasome inhibitor – Bortezomib – which is already effective in the clinical treatment of multiple myeloma and mantle lymphoma. The researchers treated Bortezomib with NPC fibroblasts with specific nonsense mutations and obtained results very similar to those obtained with two other inhibitors, ALLN and MG132.
The results obtained after using proteasome inhibitors allow the possibility of increasing the amount of NPC1 protein in the cells, in order to partially recover the functionality of NPC1.
Another proteasome inhibitor – Marizomib (NPI-0052) – which has the additional ability to cross the blood-brain barrier is in Phase II clinical trials for the treatment of multiple myeloma.
As a Conclusion
Therapeutic strategies based on the use of compounds already approved for human use facilitate access to clinical trials. This aspect would be of great importance since it would open a path to a possible mutation-addiction therapy for this disease that today has not yet been cured. In a disease as complex as Niemann-Pick type C, it is hoped that there will be to develop combined and personalized therapies according to the genotype of each patient. That is to say, it is very possible that in the future, according to the changes that a particular patient NPC presents, it is more appropriate a chosen treatment compared to another and even it could present itself the case of a combination of different therapies for the same patient.